
What is the tendon?
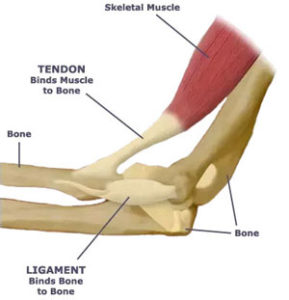
The tendon is made up of strong connective tissue found at the start (origin) and finish (insertion) of a muscle connecting the muscle to the bone ultimately allowing the muscle to contract, moving the bone and creating movement. Tendons are not to be confused with ligaments, which connect bone to bone in order to stabilise joints. Both tendons and ligaments are not elastic and are capable of withstanding incredible tensions as we walk, run, dance and jump.
(Figure taken 15/8/18 from: https://www.quora.com/What-are-t
endons-and-ligaments-and-what-are-they-composed-of)
What is a Tendinopathy?
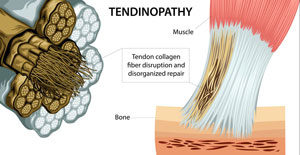
Tendonitis describes the condition in its early stages as inflammatory. After the initial stages, inflammation is no longer present and so the terminology of tendonitis should no longer be used. With tendinopathy, inflammation is no longer present. Instead, the tendon layout has been changed. When the tendon becomes overloaded by repetitive activities (e.g. jumping/running/hammering) or newly increased loading (e.g. increasing your running distance/pace dramatically), the fibres experience multiple microtraumas causing the release of inflammatory mediators. This causes the usually parallel-running tendon fibres to become disorganised. This disorganisation results in a newly thickened weaker tendon that is generally painful to touch and to load.
(Figure taken 29/8/18 from: http://chiroup.com/tendinopathy/)
Causes
- Repetitive activity – most often of energy storing activities (eg. jumping, running, hitting a tennis ball with a racquet, swinging a hammer)
- Increased loading
- Overuse
- Prolonged compressive force on the tendon
Signs & Symptoms
- Pain over the region of the tendon
- Pain extending into the muscle belly of the tendon
- Reduced strength
- Pain with contraction of the muscle (especially with energy storing activities)
- Tendon thickening
- Start-up pain with activity that can subside after a short amount of time during the activity
How to treat it?
Rest is not the cure – While symptoms subside during periods of rest, tendinopathies do not resolve and symptoms resume as activity resumes.
Exercise – Evidence tells us that exercise is one of the most effective way to treat a tendinopathy. Properly prescribed exercises aim to progressively load the tendon as tolerated in order to restore strength and reduce pain.
Shockwave therapy – Newly emerging evidence supports the use of shockwave therapy for stubborn tendinopathies (especially for insertional achilles and gluteus medius tendiopathies) (Al-Abbad & Simon, 2013; Rompe et al, 2009 & 2008; Rasmussen, et al, 2008)
Avoid aggravating activities. Avoid stretching.
References:
Abate M, Gravare-Silbernagel K, Siljeholm C, et al.: Pathogenesis of tendinopathies: inflammation or degeneration? Arthritis Research and Therapy. 2009, 11:235.
Al-Abbad, H., & Simon, J. V. (2013). The effectiveness of extracorporeal shock wave therapy on chronic achilles tendinopathy: a systematic review. Foot & ankle international,34(1), 33-41.
Cook J, Purdam C: Is compressive load a factor in the development of tendinopathy? British Journal of Sports Medicine. 2012, 46:163-168.
Malliaras P, Barton CJ, Reeves ND, Langberg H: Achilles and Patellar Tendinopathy Loading Programmes. Sports Medicine. 2013:1-20.
Rasmussen, S., Christensen, M., Mathiesen, I., & Simonson, O. (2008). Shockwave therapy for chronic Achilles tendinopathy: a double-blind, randomized clinical trial of efficacy. Acta orthopaedica, 79(2), 249-256.
Rompe, J. D., Furia, J., & Maffulli, N. (2009). Eccentric loading versus eccentric loading plus shock-wave treatment for midportion achilles tendinopathy: a randomized controlled trial.The American journal of sports medicine, 37(3), 463-470.
Rompe, J. D., Furia, J., & Maffulli, N. (2008). Eccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy: a randomized, controlled trial. JBJS,90(1), 52-61.

Recent Comments