
Anatomy of the Ankle & Foot
The anatomy of the ankle and foot area is quite complex. The ankle (a.k.a. the talocrural joint) is formed in the region where 3 bones meet: the tibia (or shin-bone), the fibular and the talus (fig. 1). The the bony knobs on either side of your ankle are formed by the tibia and fibula. These are called the medial malleolus (tibia) and lateral malleolus (fibula). The talus acts to transfer weight from the leg onto the bones in the feet, including the heel bones (calcaneus). The joint between the talus and the calcaneus is called the subtalar joint.
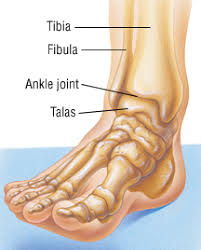
(Figure 1 – The Talocrural Joint – retrieved 23/10/18 from https://www.drugs.com/health-guide/ankle-fracture.html)
Movements created at the talocrural joint include plantar flexion and dorsiflexion. Sideways movements, known as inversion (supination) or eversion (pronation), come from the subtalar joint. These movement are demonstrated in the figure below.
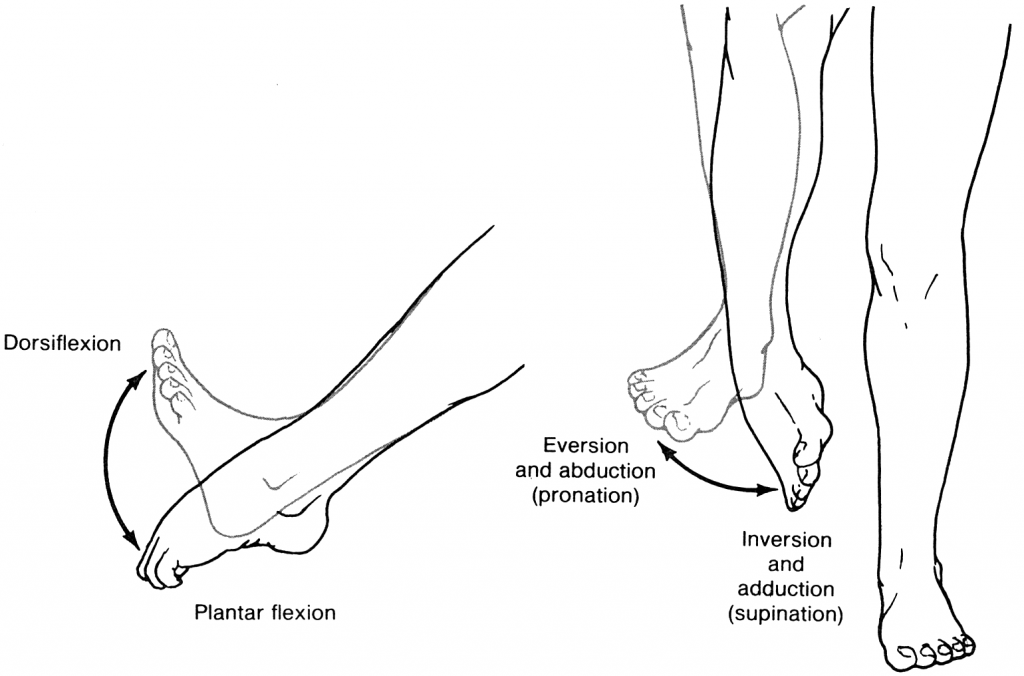
(Figure 2 – Ankle Movements. Retrieved 23/10/18 from https://accessphysiotherapy.mhmedical.com/Content.aspx?bookId=965§ionId=53599846)
Ligaments & Sprains
The ankle is secured by surrounding ligaments which support the joint. Some of these ligaments are either partially or completely torn when the ankle stretches beyond its normal range of movement (shown above). This damage to the ligament is called a sprain. The most common non-contact injury seen at the ankle occurs when someone “rolls” into inversion, stretching the ligaments on the outside of the ankle (Fig 3). This is known as an inversion injury or lateral ankle sprain. Whilst the medial ankle ligaments (Fig.4) can also be sprained through an eversion injury, these types of injuries are less common and often are a result of a more traumatic or contact-related accident.
Another less common ankle sprain occurs between the tibia and fibular (Fig. 5), known as a high ankle sprain.
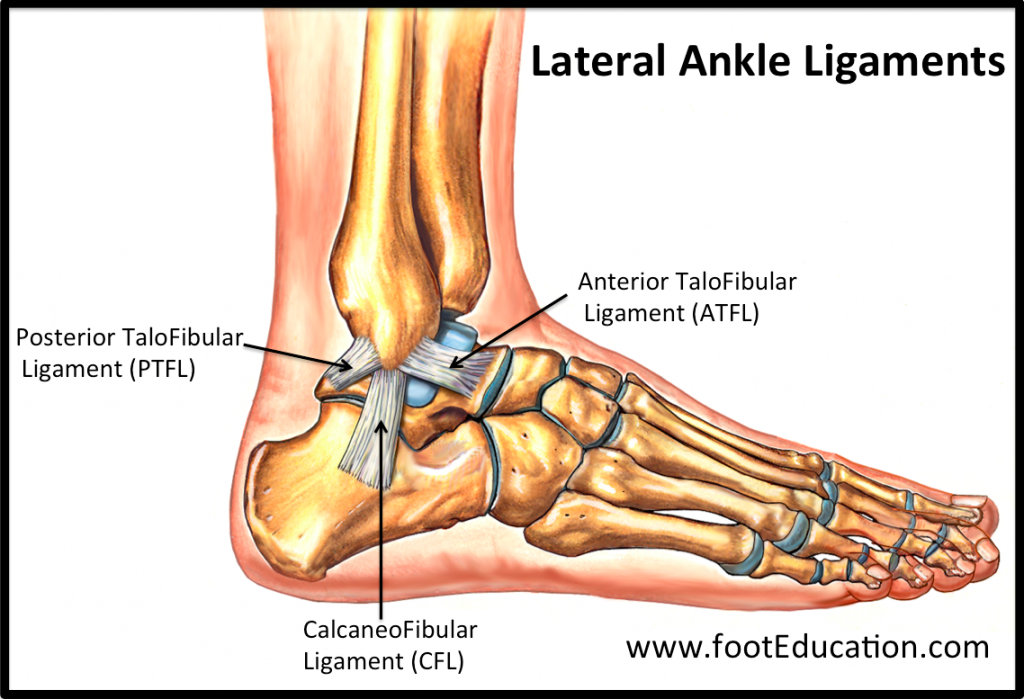
(Figure 3 – Lateral Ankle Ligaments. Retrieved 24/10/18 from https://www.footeducation.com/page/ligaments-of-foot-and-ankle-overview)
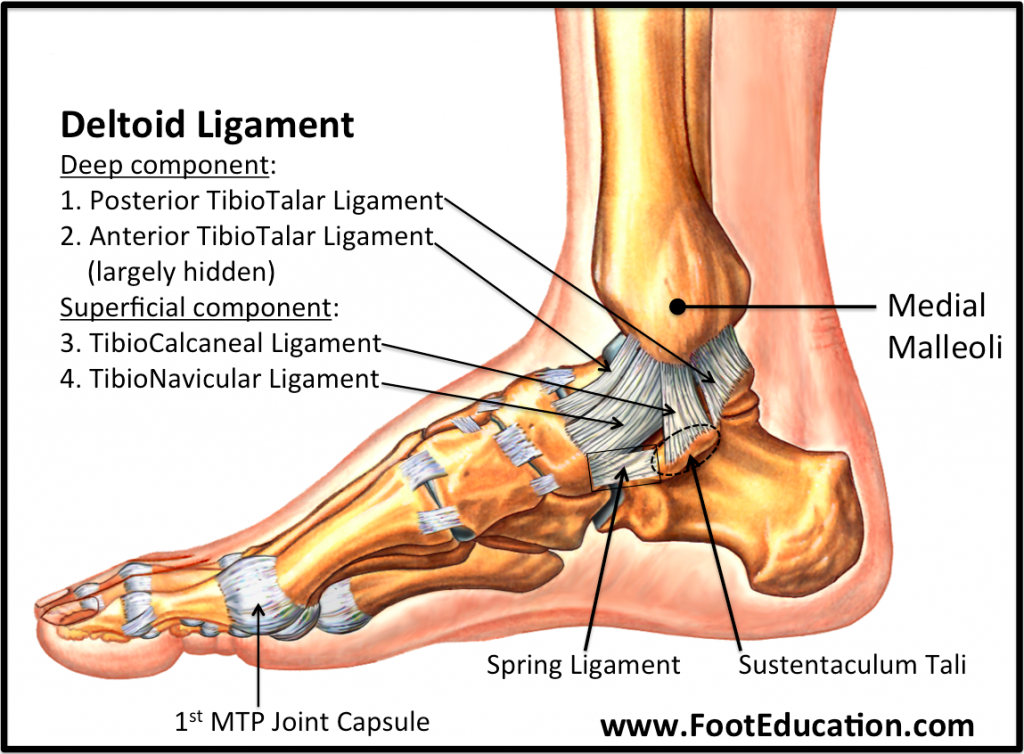
(Figure 4 – Medial Ankle Ligaments. Retrieved 24/10/18 from https://www.footeducation.com/page/ligaments-of-foot-and-ankle-overview)
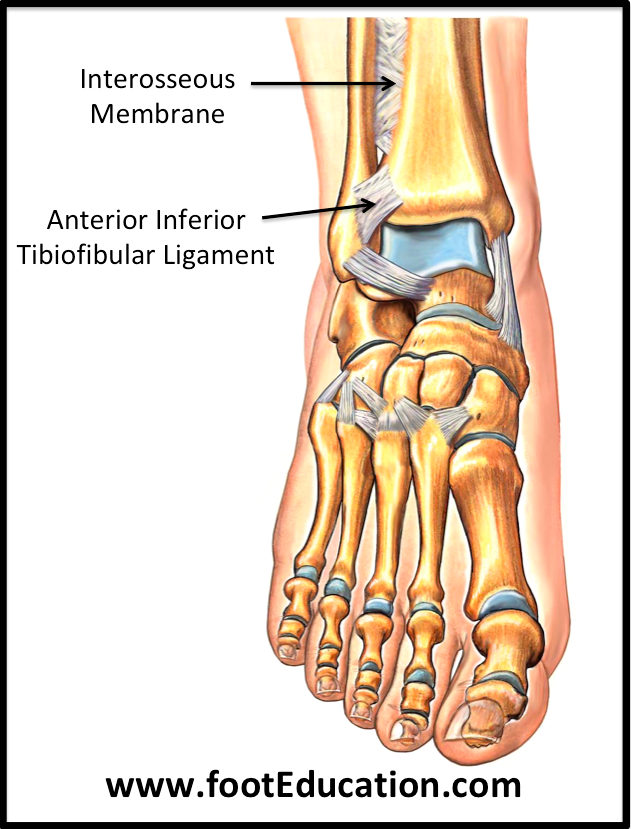
(Figure 5 – High Ankle Ligaments. Retrieved 24/10/18 from https://www.footeducation.com/page/ligaments-of-foot-and-ankle-overview)
Sprains are categorised by the severity of the damage done to the ligament, as demonstrated in Figure 6 below. Higher grades are usually associated with an increase in swelling, redness, pain, heat and loss of function (the 5 cardinal signs of inflammation – mentioned and further explained in the inflammation post below). Grade III sprains often result in joint instability/laxity. Fractures within the ankle may also be possible, depending on the severity of the sprain.
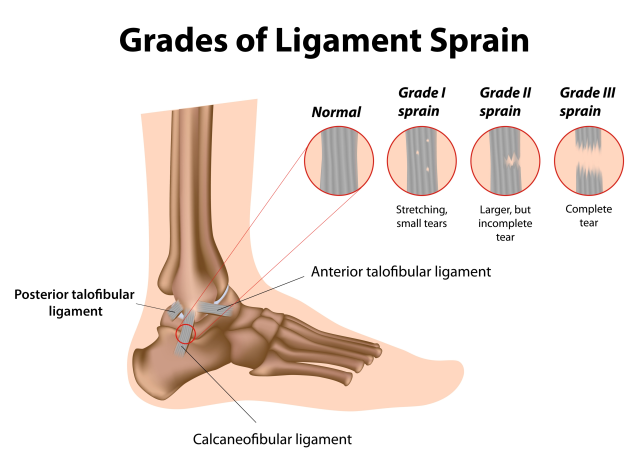
(Figure 6 – Ligament Sprain Grades. Retrieved 26/10/18 from https://www.google.com.au/url?sa=i&source=images&cd=&ved=2ahUKEwifh9bng6PeAhVCXCsKHdwgAQkQjxx6BAgBEAI&url=https%3A%2F%2Fwww.painmanagementdoctornyc.com%2Fnyc-ankle-sprain-specialist-sports-medicine-doctors%2F&psig=AOvVaw0QQISenbpHg3UZuWPYGAdK&ust=1540444976548806)
Treatment
Immediate
Historically, ankle sprains were initially treated with the R.I.C.E (Rest, Ice, Compression & Elevation) protocol. This has now evolved to M.C.E (Movement, Compression, Elevation) as a result of more research (further explained in the below post regarding inflammation). While ice may be applied immediately after the injury to help to numb the area, the emphasis of immediate management should be on applying compression to the joint, as well as elevation to help mediate swelling and safe movement, and avoid loss of function. During this phase, your physiotherapist can help to establish a safe movement pattern, unloading strategies, as well as potentially apply LAZER to assist with the management of pain and swelling.
Later
After the first week, the inflammatory stage will have ceased and the ligaments will be attempting to heal as the swelling dissipates. In this phase, the focus will be on regaining movement in a safe and gradual way. Your physiotherapist will apply manual techniques such as joint mobilisations, soft tissue release, oedema control and prescription of specific exercises aimed at reducing stiffness and improving movement within the joint. During this time, attention may also be paid to correct any compensatory mechanisms that may have arisen as a result of the injury.
It is always best to seek guidance from a trained physiotherapist to ensure a safe and appropriate recovery from an ankle sprain of any grade.

Recent Comments