
27.11.2018
Knee Osteoarthritis
What is Osteoarthritis?
Osteoarthritis (OA) is joint issue most commonly affecting a majority of the population by the age of 65 years-old (Felson, 1988). Osteoarthritis can affect any joint in the body, but one of the most common areas affected is the knee.
Often described as general wear-and-tear, osteoarthritis involves the degeneration of the bony surfaces of the knee:
- The cartilage covering degenerates to expose underlying bone
- Bony spurs (known as osteophytes) form on the inside and edges of the joint
- Ligaments and the meniscus may also deteriorate as a result being rubbed between the rough surfaces
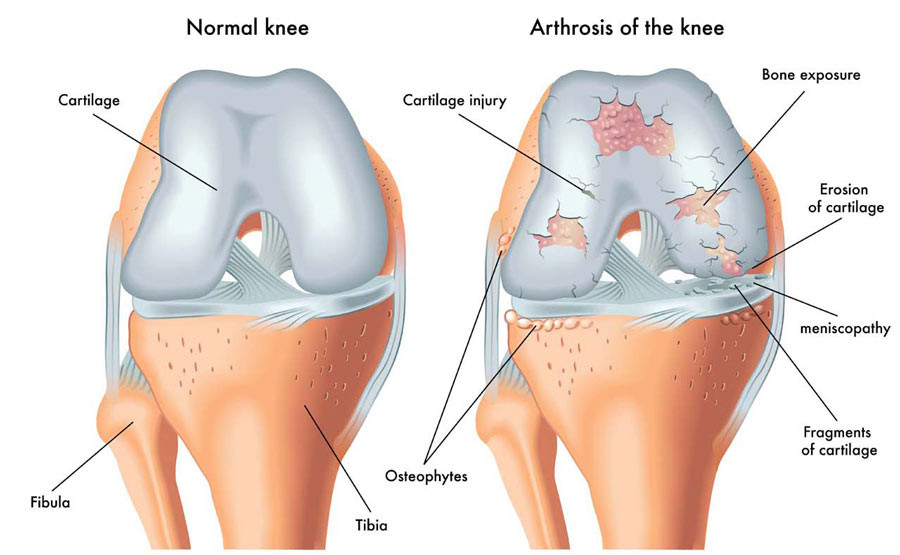
(Figure 1 – retrieved 23.11.18 from https://therapia.com/conditions/physiotherapy-for-osteoarthritis/)
This degeneration can limit movement and cause significant pain resulting in disability as the disease progresses.
Signs & Symptoms:
- Generally a slow, gradual onset of symptoms
- Deep aching pain felt felt at rest
- Increased pain with weight-bearing and with movement
- Stiffness with movement
- Crepitus (felt as creaking sensations within the joint)
- Swelling
- Deformity
- Loss of joint space as seen on an x-ray (Fig. 2)
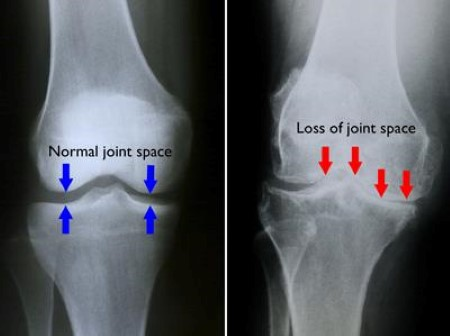
(Figure 2 – retrieved 23.11.18 from https://orthoinfo.aaos.org/en/diseases–conditions/arthritis-of-the-knee/)
Causes:
- Being overweight, which increases the force on the knee, causing more damage to the joint
- Excessive and repeated bending forces through the knee over a long period of time
- History of injury or insult to the knee
What’s the difference between Osteoarthritis and Osteoporosis?
Whilst the terms “osteoarthritis” and “osteoporosis” are often used interchangeably, they are not to be mistaken as the same condition. Osteoarthritis affects the particular surfaces of a joint as previously explained. Osteoporosis affects the inner porous matrix of the bone. Osteoporosis is the resulting dysfunction of the rate that new bone is deposited due to age related issue related to hormones, genetics, age or decreased physical activity. This lack of new bone being deposited means the bone becomes fragile and is susceptible to breaking more easily. Unlike osteoarthritis, there are no symptoms of pain or loss of function in the development of osteoporosis until a fracture occurs.
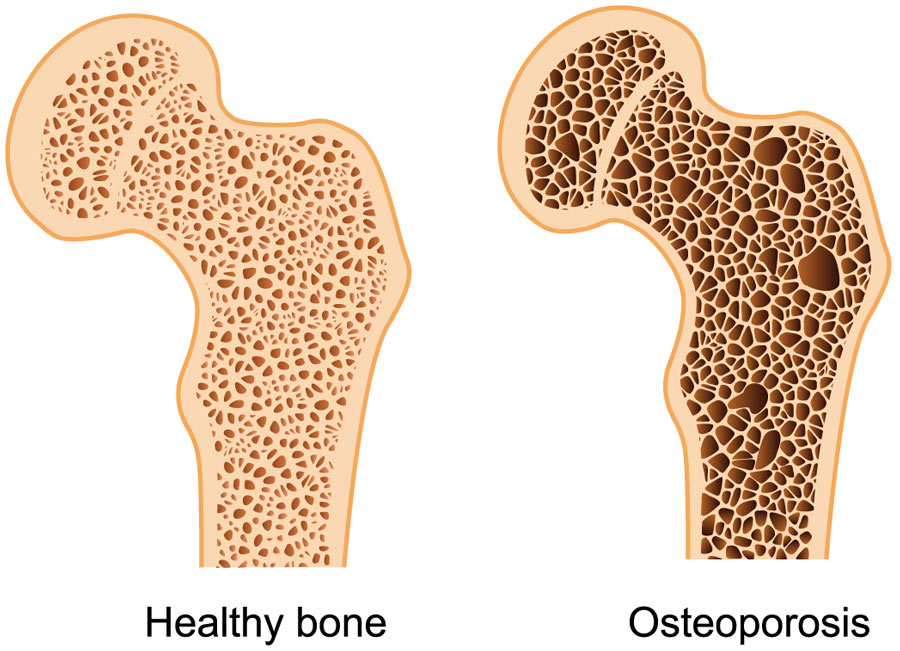
(Figure 3 – retrieved 23.11.18 – https://therapia.com/conditions/physiotherapy-for-osteoporosis/)
Treatment:
Treatment of osteoarthritis is directed at managing symptoms and enhancing or maintaining range of motion and mobility.
Conservative management
- Lifestyle change such as avoiding aggravating and high impact activities, as well as lowering body weight through diet and physical activity will reduce the forces placed through the joint, positively influencing pain and further aggravation of the joint.
- Medications such as non-steroidal anti-inflammatory or other pain relief may be prescribed by your doctor depending on the patient’s medical history.
- Heat or ice may help to reduce the sensation of pain.
- Braces and bands may provide the knee with a subjective feeling of support.
Physiotherapy treatments focusing on improving range of motion and releasing soft tissue around the knee can positively influence symptoms. Also implementing a tailored exercise program aimed at improving the strength, flexibility and proprioception (neuromuscular feedback of where the knee is as it moves) of the knee has been shown to be one of the most effective ways to reduce painful osteoarthritis symptoms, improve range and subsequently improve quality of life (Fransen & McConnell, 2008). Hydrotherapy has been demonstrated to also improve pain (Silva et al, 2008) and reduce load through the knee whilst weight-bearing, allowing the individual the opportunity to be physically active.
Surgery
- A total knee replacement may be necessary for suitable patients who have severe osteoarthritis and have genuinely attempted conservative management for many months with no improvement or worsening of symptoms.
If you experience osteoarthritis related knee pain or are aware of your progressing osteoarthritis and would like to get on top of your symptoms before they get on top of you, get in touch with a physiotherapist to start your journey of maintaining pain-free mobility throughout life.
References:
Felson; D.T. (1988) Epidemiology of hip and knee osteoarthritis, Epidemiologic Reviews, Volume 10, Issue 1, Pages 1–28
Fransen, M., & McConnell, S. (2008). Exercise for osteoarthritis of the knee. Cochrane database of systematic reviews, (4).
Silva, L. E., Valim, V., Pessanha, A. P. C., Oliveira, L. M., Myamoto, S., Jones, A., & Natour, J. (2008). Hydrotherapy versus conventional land-based exercise for the management of patients with osteoarthritis of the knee: a randomized clinical trial. Physical therapy, 88(1), 12-21.

Anatomy of the Ankle & Foot
The anatomy of the ankle and foot area is quite complex. The ankle (a.k.a. the talocrural joint) is formed in the region where 3 bones meet: the tibia (or shin-bone), the fibular and the talus (fig. 1). The the bony knobs on either side of your ankle are formed by the tibia and fibula. These are called the medial malleolus (tibia) and lateral malleolus (fibula). The talus acts to transfer weight from the leg onto the bones in the feet, including the heel bones (calcaneus). The joint between the talus and the calcaneus is called the subtalar joint.
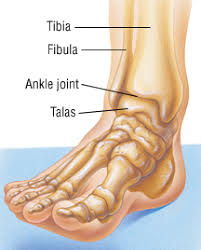
(Figure 1 – The Talocrural Joint – retrieved 23/10/18 from https://www.drugs.com/health-guide/ankle-fracture.html)
Movements created at the talocrural joint include plantar flexion and dorsiflexion. Sideways movements, known as inversion (supination) or eversion (pronation), come from the subtalar joint. These movement are demonstrated in the figure below.
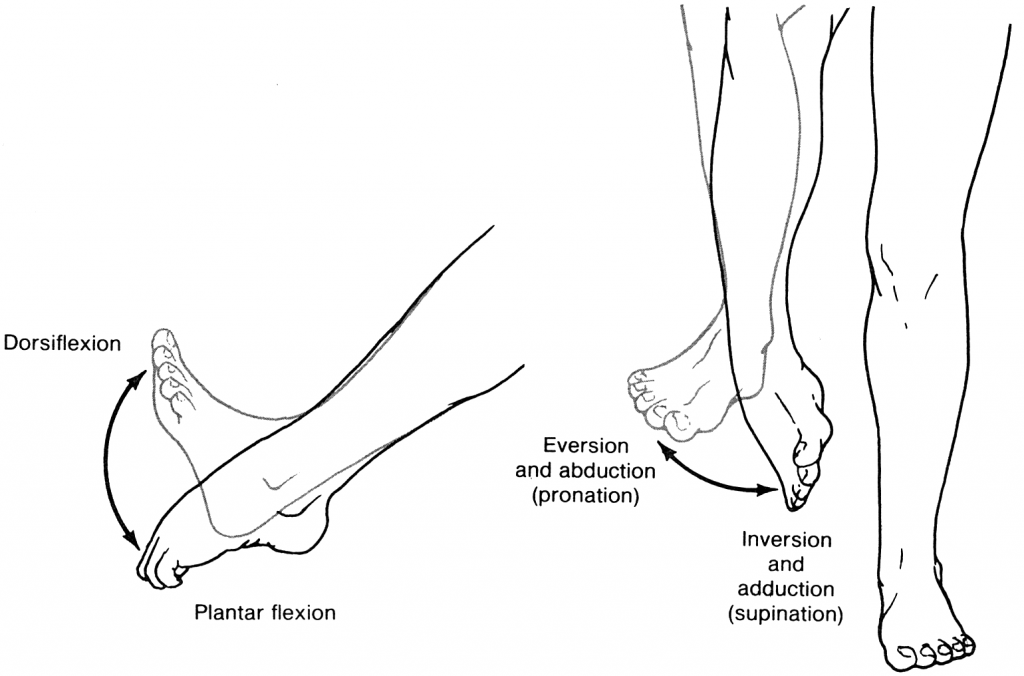
(Figure 2 – Ankle Movements. Retrieved 23/10/18 from https://accessphysiotherapy.mhmedical.com/Content.aspx?bookId=965§ionId=53599846)
Ligaments & Sprains
The ankle is secured by surrounding ligaments which support the joint. Some of these ligaments are either partially or completely torn when the ankle stretches beyond its normal range of movement (shown above). This damage to the ligament is called a sprain. The most common non-contact injury seen at the ankle occurs when someone “rolls” into inversion, stretching the ligaments on the outside of the ankle (Fig 3). This is known as an inversion injury or lateral ankle sprain. Whilst the medial ankle ligaments (Fig.4) can also be sprained through an eversion injury, these types of injuries are less common and often are a result of a more traumatic or contact-related accident.
Another less common ankle sprain occurs between the tibia and fibular (Fig. 5), known as a high ankle sprain.
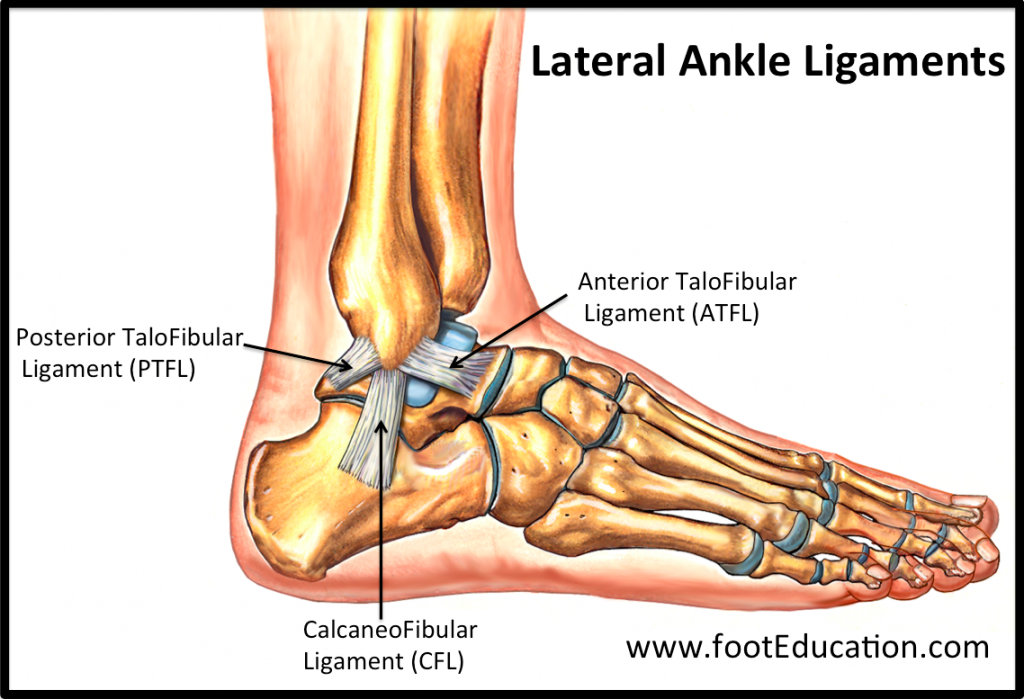
(Figure 3 – Lateral Ankle Ligaments. Retrieved 24/10/18 from https://www.footeducation.com/page/ligaments-of-foot-and-ankle-overview)
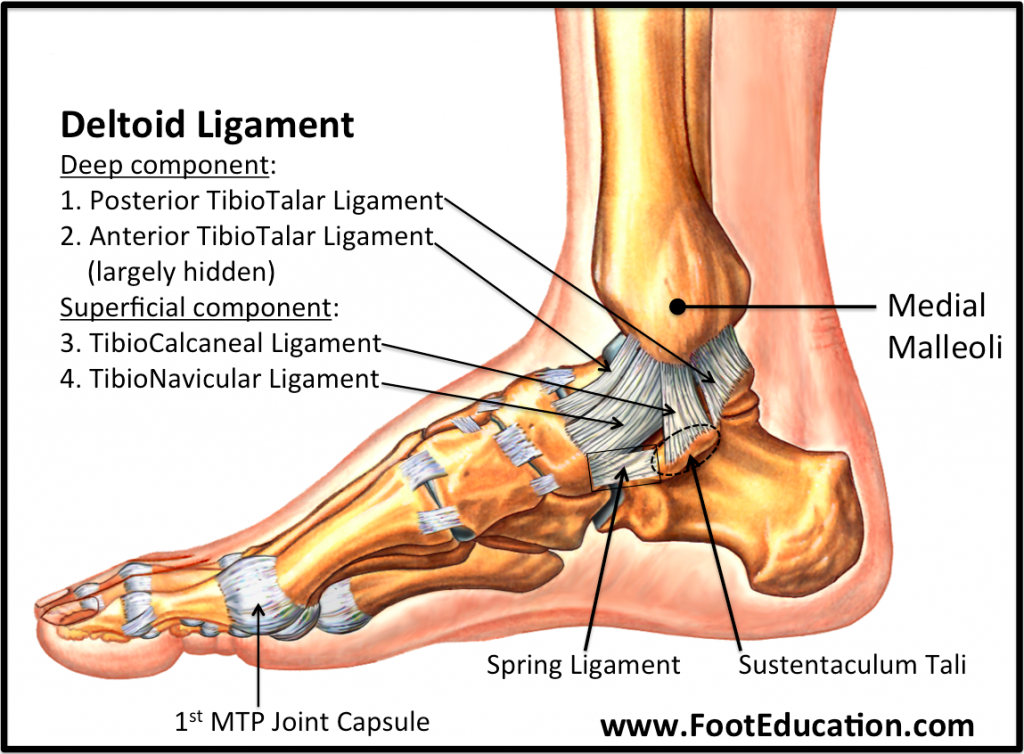
(Figure 4 – Medial Ankle Ligaments. Retrieved 24/10/18 from https://www.footeducation.com/page/ligaments-of-foot-and-ankle-overview)
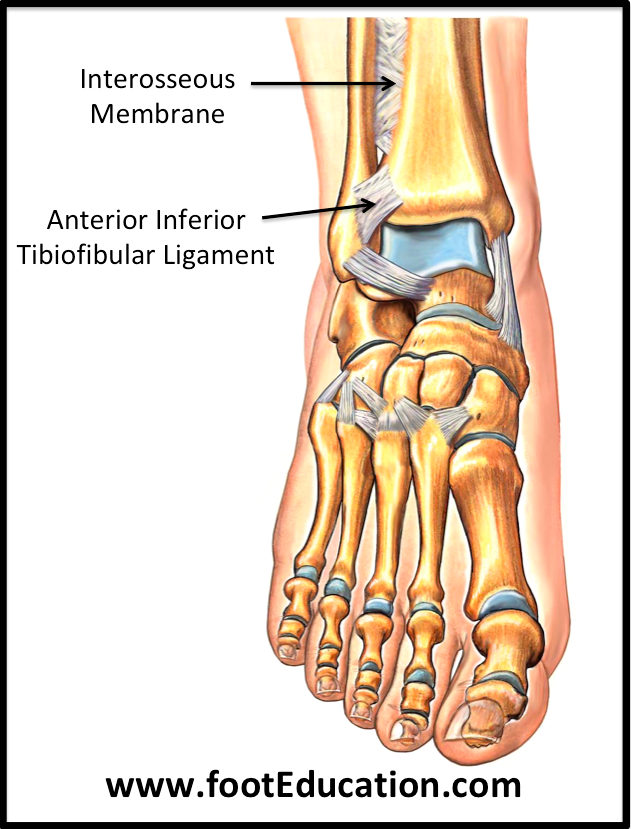
(Figure 5 – High Ankle Ligaments. Retrieved 24/10/18 from https://www.footeducation.com/page/ligaments-of-foot-and-ankle-overview)
Sprains are categorised by the severity of the damage done to the ligament, as demonstrated in Figure 6 below. Higher grades are usually associated with an increase in swelling, redness, pain, heat and loss of function (the 5 cardinal signs of inflammation – mentioned and further explained in the inflammation post below). Grade III sprains often result in joint instability/laxity. Fractures within the ankle may also be possible, depending on the severity of the sprain.
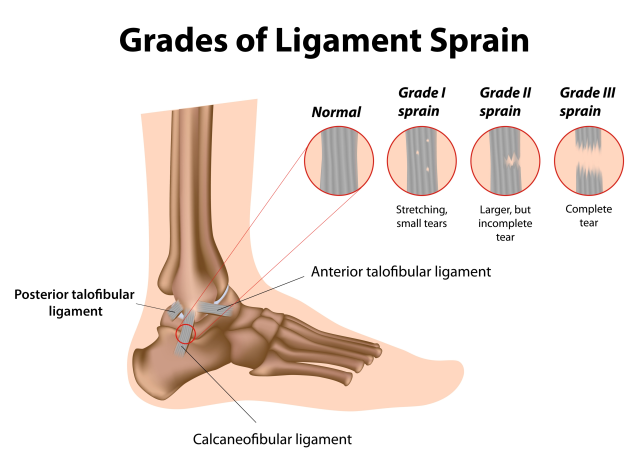
(Figure 6 – Ligament Sprain Grades. Retrieved 26/10/18 from https://www.google.com.au/url?sa=i&source=images&cd=&ved=2ahUKEwifh9bng6PeAhVCXCsKHdwgAQkQjxx6BAgBEAI&url=https%3A%2F%2Fwww.painmanagementdoctornyc.com%2Fnyc-ankle-sprain-specialist-sports-medicine-doctors%2F&psig=AOvVaw0QQISenbpHg3UZuWPYGAdK&ust=1540444976548806)
Treatment
Immediate
Historically, ankle sprains were initially treated with the R.I.C.E (Rest, Ice, Compression & Elevation) protocol. This has now evolved to M.C.E (Movement, Compression, Elevation) as a result of more research (further explained in the below post regarding inflammation). While ice may be applied immediately after the injury to help to numb the area, the emphasis of immediate management should be on applying compression to the joint, as well as elevation to help mediate swelling and safe movement, and avoid loss of function. During this phase, your physiotherapist can help to establish a safe movement pattern, unloading strategies, as well as potentially apply LAZER to assist with the management of pain and swelling.
Later
After the first week, the inflammatory stage will have ceased and the ligaments will be attempting to heal as the swelling dissipates. In this phase, the focus will be on regaining movement in a safe and gradual way. Your physiotherapist will apply manual techniques such as joint mobilisations, soft tissue release, oedema control and prescription of specific exercises aimed at reducing stiffness and improving movement within the joint. During this time, attention may also be paid to correct any compensatory mechanisms that may have arisen as a result of the injury.
It is always best to seek guidance from a trained physiotherapist to ensure a safe and appropriate recovery from an ankle sprain of any grade.

08.11.2018
Abel Tasman National Park
From October 21 to October 28, 20 clients and friends of Bangalow Physiotherapy travelled to Abel Tasman National Park for a 50km hike. We had a lovely time with minimal injuries, before being wined, dined and guided by the ever-so-gracious Wilson Abel Tasman. For two nights, we stayed in two different locations as we “stamped” our way through the park.
We were initially ferried to our starting location, passing some adorable seals sunning themselves on an island. We also enjoyed the native birdlife on offer in the park.
On two different days, in two different locations, some of us took up kayaking in the glorious estuaries – others decided to sea kayak (with plenty more sightings of seals). And some of us simply enjoyed the tranquil offerings of the local walking tracks. A wonderful trip to remember.

Awaroa Bay

Torrent Bay Lodge – view from the track

Kim at Cleopatra’s Pool
Beach near Torrent Bay





Recent Comments